#image_title
#image_title
Got questions? We’ve got answers.
After over a year of staying at home due to the COVID-19 pandemic, there is something in 2021 that has established a glimmer of hope, a light at the end of the tunnel: a vaccine.
But it can only work as hard as the population that is willing to put it to good use.
The trend is going in the right direction, but make no mistake—COVID-19 continues to spread in Wisconsin and beyond. More than 131,000 Wisconsinites were diagnosed with COVID-19 in 2021, and more than 1,400 people in the state have died from the virus in the first six months of the new year. Nationally, the new year has already brought about 13 million new infections and over 245,000 deaths.
There have now been about 612,000 confirmed coronavirus cases in Wisconsin since the pandemic arrived last March and over 7,200 deaths; nationally, there are over 33.5 million cases and more than 600,000 deaths.
While America’s response to the pandemic was initially nothing short of a disaster, the scientific and medical community managed to deliver three vaccines—Moderna, Pfizer, and Johnson & Johnson—and new virus cases have declined as more resources have been distributed and vaccines have become widely available.
Where can I get the vaccine?
Visit https://www.vaccines.gov/search/ or call 211 to find vaccine availability with options to filter location or the specific type of vaccine (Pfizer, Moderna, or J&J). Employers, local/tribal health departments, pharmacies, or health care providers may offer vaccinations at no cost, as well as community-based or pop-up vaccination clinics. Many mass vaccination hubs that were open from the start, like the one at the Wisconsin Center in Milwaukee, are now closing in favor of opening smaller, more localized vaccination clinics to increase accessibility, particularly in rural areas.
From now through July 4, Uber and Lyft are offering free or discounted rides to those who need transportation to and from their vaccine appointments. Uber is offering up to four rides (up to $25 per ride), and Lyft is offering up to two rides (up to $15 per ride). Users can access these discounts through the Uber app and the Lyft website.
As demand is declining for vaccinations, many locations are beginning to accept walk-ins so that doses don’t go to waste.
What does the vaccine cost? Do I need insurance or American citizenship?
Nothing. Vaccines are free for everyone, even without insurance.
Immigration status also is not a factor in qualifying for a vaccine. Although a social security number or government ID may be requested at a vaccination site, it is not required.
How many COVID vaccines are there, and how many will there be?
While much has been said about the first approved vaccines, there are actually dozens of other vaccines in various stages of development. More than 100 vaccines are in trials, eight are in early or limited use, and eight are in full use, according to a New York Times database.
Americans began receiving the Pfizer vaccine in mid-December after it was first to receive approval from the federal Food and Drug Administration for an Emergency Use Authorization (EUA). Pfizer partnered with the German company BioNTech on its vaccine.
The FDA authorized the Pfizer vaccine for use to anyone 12 years of age or older as of May 10.
Moderna’s vaccine started to roll out about a week later. It was developed in partnership with the National Institutes of Health. It is still only available for adults 18 and older.
Clinical trials found better than 90% efficacy in both vaccines, which are delivered in two shots three and four weeks apart, respectively.
The FDA approved Johnson & Johnson’s single-dose vaccine at the end of February for those 18 years and older. This vaccine has 66% efficacy, and part of its clinical trial took place in South Africa where the Beta variant was already spreading. Infectious disease experts emphasized that its efficacy should not be compared to the Pfizer and Moderna vaccines as they held their clinical trials earlier when fewer infections and variants were spreading, among other variables.
How many people have gotten vaccinated?
Wisconsin’s vaccine rollout was plagued with issues at the start, not the least of which was a low supply of doses sent by the federal government, according to the state Department of Health Services (DHS) and Gov. Tony Evers.
Nonetheless, the state’s rollout recovered and more than 5.4 million doses have been administered in Wisconsin as of June 18, according to DHS. Providers have administered over 2.2 million doses of the Moderna vaccine, almost 3 million of the Pfizer vaccine, and over 220,000 of the Johnson & Johnson vaccine to Wisconsinites.
Although demand for the vaccine was high initially, Wisconsin’s vaccination rate has plateaued, still short of 50% of the population having received at least one dose.
RELATED: DHS Launches New COVID-19 Vaccination Campaign to Reach Young Adults
About 175 million Americans have received their first dose, according to the Centers for Disease Control and Prevention. Over 375 million doses have been distributed around the country.
Nearly 53% of Americans have received their first dose. President Biden is aiming to have 70% of US adults with at least one dose by July 4.
Wisconsin’s goal is to achieve herd immunity through an 80% or higher vaccination level to “keep us all safe and get back to the things we love.”
Who is getting vaccines right now?
Back in early March, President Biden called to have vaccines available for every US adult by the end of May, and eventually he moved the deadline even earlier to the 1st of May. Ultimately, on April 19, all US adults became eligible in all 50 states, DC, and Puerto Rico to receive the COVID-19 vaccine, surpassing Biden’s timeline by 11 days.
Wisconsin’s vaccine rollout began with frontline workers such as healthcare providers and the residents and staff of skilled nursing facilities back in mid-December of 2020. On Jan. 18, eligibility opened to firefighters, police, and EMTs. Adults 65 and older could get their vaccine starting Jan. 25. The next large phase of the rollout included education and child care workers, individuals enrolled in Medicaid long-term care programs, non-frontline health care essential personnel, facility staff and residents in congregate living settings, and other essential workers, which opened on Mar. 1. Wisconsinites with medical conditions that put them at higher risk of contracting COVID-19 could get their vaccine as early as March 22, a week earlier than the state’s anticipated timeline.
Evers originally didn’t anticipate general eligibility until May or June, but everyone in the state 16 years or older was made eligible to get the vaccine on April 5. More recently, as of May 13, 12-15 year-olds can now receive their vaccine after the FDA authorized the Pfizer vaccine for emergency use for this new age group.
Is the vaccine safe?
The vaccine development process is a rigorous, comprehensive process that begins with testing a new vaccine on animals, such as mice or monkeys, to see if it produces an immune response. Scientists then give the vaccine to humans in three separate phases, beginning with a small number of people in phase one in order to test safety and dosage and determine if it triggers the immune system. In phase two, scientists give the vaccine to hundreds of people across different age ranges and at different levels of health, in order to see how the vaccine behaves among different populations. In the third and final phase, tens of thousands of people receive the vaccine, and scientists compare their health outcomes with test subjects who received a placebo. This effectively shows whether the vaccine protects against COVID-19 and whether the vaccines produce any rare or dangerous side effects.
The process is thorough and the bar to clear for FDA approval is high, incentivizing companies to take a safe, conservative approach. Multiple companies, including AstraZeneca—which conducted its trials in partnership with Oxford University—and Johnson & Johnson temporarily paused their COVID vaccine trials to investigate potentially adverse side effects in one person in each trial, before ultimately resuming them after the unexpected illnesses could not be linked to the vaccines.
Since these current FDA-approved vaccines have been authorized for emergency use, there has been some confusion over whether the testing, research, and clinical studies were less rigorous than the normal authorization process. However, this is not the case.
The only difference between regular authorization and EUA is that under EUA, production of the vaccine occurs simultaneously alongside the testing phase rather than occurring after approval of the vaccine in a non-emergent scenario.
According to University of North Carolina Health’s COVID-19 Vaccine Hub, “An EUA does not affect vaccine safety, because it does not impact development, such as research, clinical studies and the studying of side effects and adverse reactions. Instead, it speeds up manufacturing and administrative processes.”
As part of their applications to the FDA, both Moderna and Pfizer included two months of follow-up safety data from their Phase 3 human clinical trials that were conducted by independent bodies, such as universities. By September, Pfizer had enrolled 44,000 participants in its trial without a single serious safety issue being reported.
Some trial participants and vaccine recipients have experienced side effects, including fever, muscle aches, headaches, and fatigue after receiving the shots, but those symptoms generally did not last more than a day. Such reactions are usually a sign that the body’s immune response is being activated as intended.
It’s rare, but some vaccine recipients, including a frontline worker in Oshkosh, have experienced severe side effects stemming from allergic reactions. The CDC estimates about one in 90,000 people will experience a severe allergic reaction.
On April 13, the CDC and FDA called for a pause of the J&J vaccine upon receiving six reports of women developing blood clots following their vaccinations. Although this was just 0.0001% of people who received this vaccine in the US, health officials wanted to err on the side of caution to ensure the safety of those getting vaccinated. The agencies lifted the pause 10 days later on April 23 after releasing new fact sheets with additional information on the risk of blood clots associated with the vaccine.
Politics
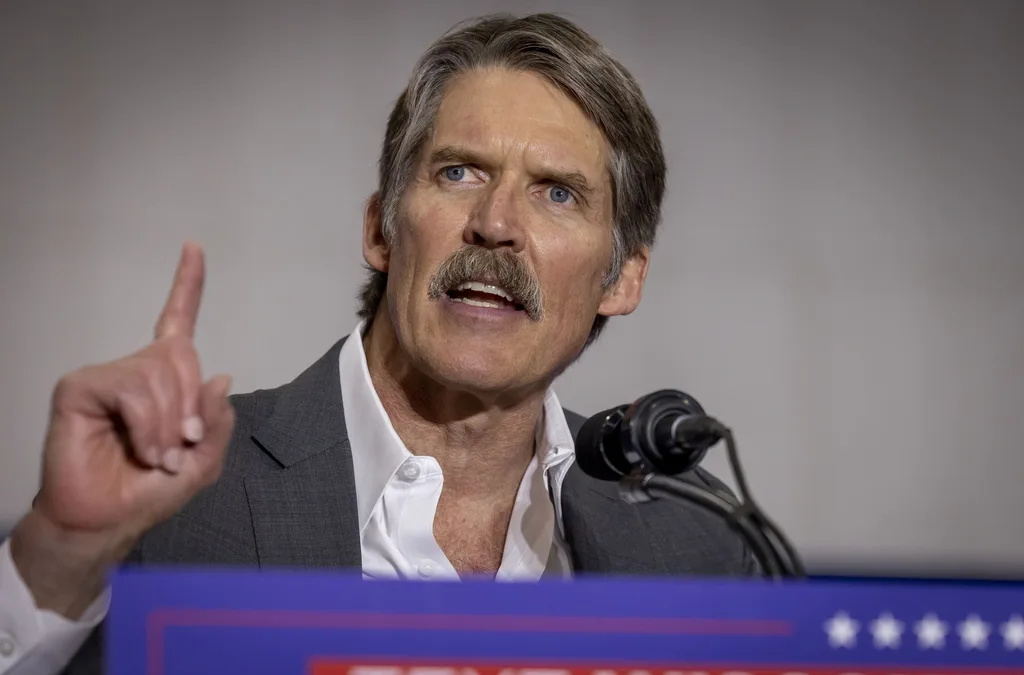
Eric Hovde’s company exposed workers to dangerous chemicals, OSHA reports say
A Madison-based real estate company run by Wisconsin US Senate candidate Eric Hovde settled with the Occupational Safety and Health Administration...

Plugged in: How one Wisconsin school bus driver likes his new electric bus
Electric school buses are gradually being rolled out across the state. They’re still big and yellow, but they’re not loud and don’t smell like...
Local News

Stop and smell these native Wisconsin flowers this Earth Day
Spring has sprung — and here in Wisconsin, the signs are everywhere! From warmer weather and longer days to birds returning to your backyard trees....

Your guide to the 2024 Blue Ox Music Festival in Eau Claire
Eau Claire and art go hand in hand. The city is home to a multitude of sculptures, murals, and music events — including several annual showcases,...