#image_title
#image_title
Current fight to contain this surge is described as “new and dangerous,” ”pivotal,” “critical.”
The state of Wisconsin is entering a new phase in its battle against the coronavirus, and it’s not winning the fight, especially in rural Wisconsin.
“I don’t think what we are experiencing is the second or third surge,” Dr. Mark Kaufman, the Wisconsin Hospital Association’s chief medical officer, told UpNorthNews in an interview Wednesday. “I think of it now as one continuous roller-coaster ride and we are climbing higher than we have ever gone before.”
On Thursday, the state continued its trend of record-setting day, after record-setting day by setting a new single-day hospitalization record of 528, up from 508 on Wednesday, according to the Wisconsin Hospital Association. This is an increase of 159 hospitalized patients from one week ago. Of the overall number of patients hospitalized, 151 are receiving care in intensive care units.
The association tracks statewide data pertaining to COVID-19 patients, the number of intensive care rooms available, and other metrics such as availability of ventilators to treat patients with severe respiratory failure. The last time hospitalized patients were near the levels they have been during this past week or so was in April when 446 people were hospitalized on April 9.
The filling of hospitals statewide correlates with the rise in overall cases across Wisconsin. On Thursday, the state saw its second-highest, single-day total, with 2,392 new cases.
“To me, the most striking pieces of information related to the spread of the coronavirus is the uptick in rural areas and the sharp increase in the rate of hospitalizations in these areas,” said Kaufman.
The hospital association quantifies data by geographical areas of the state known as health care emergency readiness coalition regions. The state has seven.
To Kaufman’s point, the southeast health care readiness region is a seven-county area that includes Milwaukee. It is the most densely populated region of the state, but its rate of increase and percent increase of hospitalized patients is the lowest. As of Tuesday, the southeast region had 178 patients hospitalized with COVID-19, up from 132 on Sept. 5.
In contrast, the rural, western region of the state that includes Buffalo, Crawford, Jackson, La Crosse, Monroe, Trempealeau, and Vernon counties has the highest rate of increases in hospitalizations. In the 24-day span between Aug. 29 and Sept. 22, the number of hospitalized coronavirus patients increased from two to 22.
Another largely rural portion of the state is the north-central region. It includes Clark, Forest, Iron, Marathon, Langlade, Lincoln, Oneida, Portage, Price, Taylor, Vilas, and Wood counties. This region saw its number of hospitalized patients more than triple in a 10-day span from 17 on Sept. 12 to 64 on Tuesday.
In the northeast region, which includes Brown, Door, Florence, Kewaunee, Manitowoc, Marinette, and Oconto counties, there has been a sixfold increase, with hospitalized patients increasing from 14 on Aug. 29 to 66 on Sept. 22.
In contrast, the southcentral region that includes 14 counties, including Dane County and the UW-Madison campus, has seen its patient hospitalization numbers remain steady at roughly 40 people hospitalized per day, Kaufman said.
“Entering into the fall is not the time to relax our precautions and our behaviors, so we need to go back a little bit to the way we were,” said Dr. Nasia Safdar, medical director for infection prevention at UW Health in Madison, referring to increased safeguards and reduced public exposure.
Ken Nelson is the chief nursing officer with HSHS St. Vincent Hospital and HSHS St. Mary’s Hospital Medical Center in Green Bay. The hospitals are part of a six-hospital system, allowing resources to be leveraged between facilities, Nelson said.
He said he remembers back to when the first coronavirus-positive patient was reported in Wisconsin.
“We’ve been planning for this day since February. We are ready,” Nelson said Thursday. “We have had the luxury of time to plan.”
Jesse Tischer, Aspirus Wausau Hospital interim president, said the region is at a “pivotal moment” in its fight against the virus.
As of Wednesday morning, Aspirus had 27 positive COVID-19 patients hospitalized across the system, with most at its Wausau hospital. That’s the largest number since the start of the pandemic, said Tischer, who’s also senior vice president and president of regional markets for the health system.
“The increases that we saw across the nation are now making it to us here,” he said. “Now is a critical time for us in central Wisconsin. Aspirus is ready.”
Health care professionals agree the increase in cases cannot be pinned solely on the behavior of college students. Every state has college campuses, but not every state is ranked as one of the worst for the increasing spread of the coronavirus.
Kaufman points to states like New York, where bars and restaurants still are not allowed to operate to the extent they are in Wisconsin. But most say the increase is due to non-compliance. People are not wearing masks, social distancing, routinely washing their hands, and avoiding large gatherings.
“There is no doubt our compliance is not at 100 percent,” Kaufman said. “I think we each need to look at ourselves and ask ourselves if we are doing everything we can individually to control the pandemic. If we each do that, things will get much better soon.”
When asked if he was surprised by the surge in hospitalized patients in the Green Bay area where he works, Nelson responded by sharing his experience from spending Wednesday with coronavirus patients and his staff in an intensive care unit.
For him, it is a mix of anger, sadness, and admiration.
“When people talk about how this is a hoax and how after the election this will be over, and how there is just this misconception about the severity, that’s the part of me that’s very angry,” he said.
He said many of his staff wear a a protective air respiratory protective device, known as a PAPR, for hours on end during their shifts to enable them to be in the same room with COVID-positive patients and not contract the virus. The device resembles an astronaut helmet. He said he saw the look in the eyes of staff as they emerged from rooms, exhausted and covered in sweat.
“All the credit in the world goes to the nurses, the nursing assistants, physicians—everybody who is doing this to take care of not only our COVID patients but everyone that needs us,” Nelson said. “It is difficult right now.”
Politics
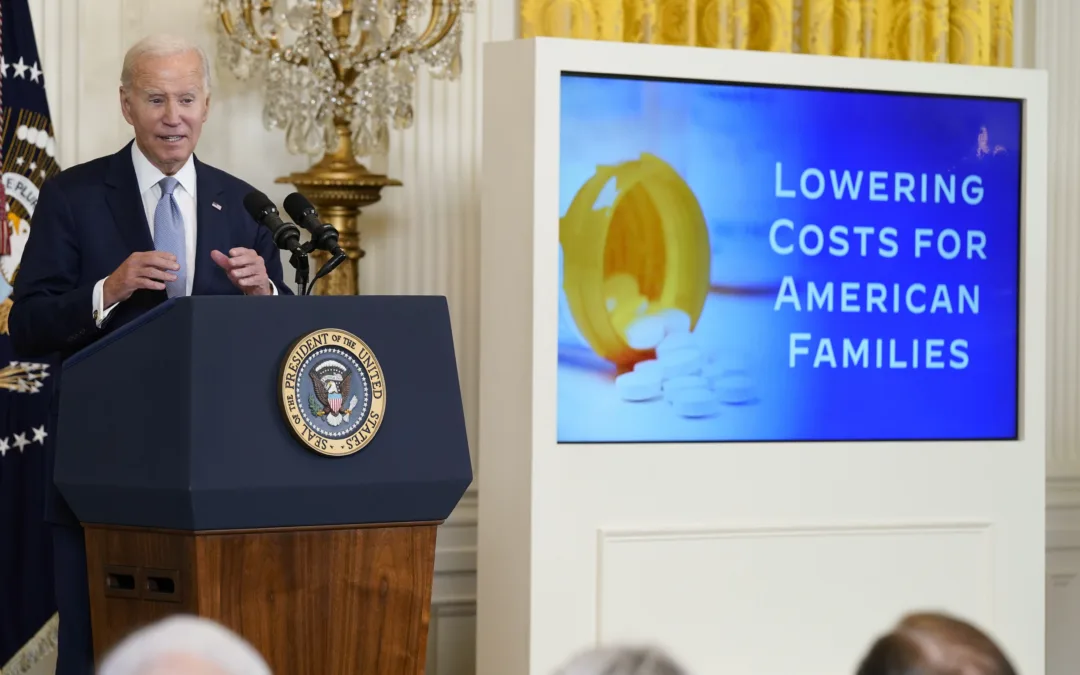
Opinion: Many reasons why young adults should refuse to let Republicans kill the Affordable Care Act
In this op-ed, University of Wisconsin Medical School student, Samantha Crowley, shares the importance of young adults protecting the Affordable...
He said what? 10 things to know about RFK Jr.
The Kennedy family has long been considered “Democratic royalty.” But Robert F. Kennedy, Jr.—son of Robert F. Kennedy, who was assassinated while...
Local News

Stop and smell these native Wisconsin flowers this Earth Day
Spring has sprung — and here in Wisconsin, the signs are everywhere! From warmer weather and longer days to birds returning to your backyard trees....

Your guide to the 2024 Blue Ox Music Festival in Eau Claire
Eau Claire and art go hand in hand. The city is home to a multitude of sculptures, murals, and music events — including several annual showcases,...