#image_title
#image_title
Mayo’s five hospitals in the northwest region are at 100% of capacity, more than 300 nurses and medical staff quarantined.
For the last eight years, Pam White has worked from her Mayo Clinic Health System office in downtown Eau Claire, where the chief nursing officer supervised nurses in Eau Claire and the four other Mayo hospitals and additional clinics scattered across northwest Wisconsin.
But on Oct. 28, White traded in her normal dress clothes for the traditional blue uniform and scrubs worn by Mayo nurses.
When she showed up to work that day, she took a selfie outside of the hospital to mark the occasion, then headed inside, where she prepared to care for patients. It’s a job she hadn’t done on a daily basis for about 20 years.
She put on personal protective gear, one piece at a time. Mask. Gown. Gloves. Face shield. Then it was time to care for her first COVID-19 patient.
White’s transition from administrator to nurse on the floor is a sign of an rapid influx of COVID-19 patients in recent weeks hospitalized at Mayo, a situation that is stressing existing resources to the breaking point and has caused a staffing shortage severe enough to send administrators like her to the front lines. Mayo’s five hospitals in the region are at 100% of capacity and more than 300 nurses and other medical staff are quarantined because of exposure to the virus.
“It’s a sign of what we’re dealing with now, with so many more cases of the virus,” White said during an interview Friday when asked about working directly with patients again. “It’s not what happens normally. But it is the right thing to do right now, and it sends my staff the right message. It’s what is needed.”
Mayo and other Wisconsin hospitals will soon be dealing with more COVID-19 patients. On Friday, Wisconsin recorded yet another one-day record number of COVID-19 cases, a total of 7,777, topping 300,000 statewide since March. Of those, more than 100,000 have been in the past 18 days.
Another 58 deaths also were reported Friday, along with 274 additional hospitalizations. The number of people requiring hospitalization because of COVID-19 has risen dramatically at Mayo’s hospitals and others across the state in recent weeks, and as of Thursday totaled 2,077.
More than 250 additional COVID patients have been hospitalized daily during the past week, stretching resources to the breaking point. Numerous hospitals in Wisconsin report being at or near patient capacity as the number of people infected with the virus keeps increasing.
One month ago, there were 26 patients hospitalized with the virus at Mayo’s northwest Wisconsin hospitals. On Friday, that number was 86. Mayo hospitals in the region are at 100% of capacity, forcing patient backups in emergency rooms until beds open up. Elective procedures are being delayed to focus available resources on COVID-19 patients.
The increased patient load comes as fewer nurses and other medical staff are available to treat them. Because of the contagious nature of the coronavirus, hospitals face significant staff shortages because their workers have been exposed to the virus and must be quarantined.
Thousands of nurses and hospital staff at Wisconsin hospitals are currently in isolation after COVID-19 exposure, stretching personnel available to care for them. That figure totals more than 300 at Mayo sites in northwest Wisconsin, White said, and prompted her and other Mayo administrators to work directly with patients.
Those fast-growing numbers and increasingly stressful work conditions are stretching the physical and emotional capabilities of nurses, White said. Extra-long work shifts, working many days straight, and doing so amid an especially contagious, potentially dangerous disease is taking a toll on nurses at Mayo and elsewhere.
“You drive by our hospital, and from the outside everything looks normal,” she said. “But things are anything but normal on the inside.”

‘Absolutely heartbreaking’
Inside, White said, nurses and other medical staff are scrambling to keep up with an ever-growing workload as staff numbers shrink with each exposure to the virus. They are especially cognizant of the potentially deadly nature of the virus as they see the damage it can do to patients firsthand.
More patients hospitalized with the virus are more sick than during previous periods of the pandemic, White said, and more of them are requiring intensive care. Dealing with patients who are seriously ill and dying while working extra-long shifts day after day is causing significant stress for nurses and other medical staff, she said.
Nurses are not only treating patients, but are taking the place of family members who can’t be at the bedsides of those hospitalized with COVID-19 because of the virus’ contagious nature. In some cases, she said, nurses are arranging the last phone calls between those dying from the virus and their loved ones. They are watching multiple members of the same family die from the virus.
During a recent conversation, White said, a longtime, experienced nurse confided that the previous day was the first in months that she hadn’t cried after finishing her work shift.
“We are handling situations here we never have before,” White said, her voice choked with emotion. “To arrange a phone call between people when you know that may be the last time they ever talk, it’s absolutely heartbreaking.”
Nurses and other medical staff across the state are experiencing similarly challenging working conditions as COVID-19 cases spike, said Eric Borgerding, chief operating officer of the Wisconsin Hospital Association. Virus exposure among hospital employees causes not only fear among others of contracting the virus but is forcing them to work extra hours to make up for their absent colleagues.
“The situation is causing difficulties all over the state,” he said.
Some hospitals are bringing in nurses from elsewhere to address a lack of staffing. Mayo is accepting help from nurses at its Arizona facilities, White said, after those from this region helped there in summer months when a surge occurred in the southwestern US. Traveling nurses also are helping fill the gap, she said, as are nurses from the Mayo site in Rochester, Minnesota.
“All of those other patient needs didn’t go away,” White said. “We still have people having heart attacks, people who need surgeries. We need all the staff we can get right now.”
Many challenges
White’s first day working directly with COVID-19 patients wasn’t easy. A registered nurse for 38 years, she knew plenty about caring for those with illnesses.
But this wasn’t just any illness, White knew. COVID-19 is especially contagious and can spread rapidly in congregate settings such as hospitals.
The disease is different from other viruses in another way. It is more deadly, and no vaccine to prevent it has yet been developed and approved.
Those thoughts, hammered home by the ample personal protective equipment she had to make sure to wear each time she interacted with someone, were a distraction at first, White said.
“I was nervous,” she recalled of that day nearly three weeks ago. “There is all of the personal protective equipment to wear, all of this other stuff to think about. You know about the risks. Then you remember there is a patient in that bed, how they need your help.”
The nurses she works with are nervous about working among COVID-19 too, White said, especially as outbreaks continue and more people are infected. They see firsthand the potential deadly impacts of the virus.
“It is very hard right now,” White said. “We try to stay positive and to stay resilient. There are just some things you have to let go.”
White praised her nurses, saying they are overcoming extremely challenging conditions to provide top-quality care. She noted their support for one another, how they help each other and remind one another of positive happenings.
White has her own method of trying to remain upbeat amid the growing challenges posed by the coronavirus. Before she heads home from work, she makes sure she writes at least three positive happenings that occurred that day.
The messages can be simple, and seem relatively uneventful to others. An upbeat comment. A positive outcome. Nice weather.
But to White, those words on a whiteboard in her office represent more than nice happenstances. They serve as uplifting rays of light amid the many difficult moments White and her fellow nurses face amid a rapidly rising number of coronavirus-related hospitalizations that are overwhelming hospitals across Wisconsin.
“It’s one thing I can do to try to stay positive,” she said.
‘Maintain hope’
The COVID-19 burden on hospitals in Wisconsin and elsewhere doesn’t appear likely to let up anytime soon. Virus-related cases, deaths, and hospitalizations are projected to continue to increase, with the number of deaths in the state projected to double to about 5,000.
The state remains among the nation’s worst COVID-19 hotspots, and public health officials worry that family gatherings for Thanksgiving and Christmas; people spending more time indoors because of cold weather; and the refusal of some to wear masks in public, practice social distancing, and refrain from gatherings, will lead to a continued surge.
“I wish I could say that we’re over the top with this,” White said, “but we’re not. That’s the scary part of this. Where will the patients go as we keep having more of them, and who will care for them?”
On Tuesday Gov. Tony Evers advised Wisconsin residents to stay home as much as possible and refrain from gathering with others in an attempt to slow the spread of the virus. Like Evers, White reiterated the need for people to wash hands often, wear a mask in public, and avoid gatherings. She recently told her family they can’t gather for Thanksgiving because of concerns about the virus.
“Whether it’s a large gathering or a small one, this virus doesn’t care about that,” White said. “This is how it spreads.”
Despite challenging, desperate moments, despite the depressing specter of illness and death around her, White said she finds hope. She finds it in the resiliency of her fellow nurses continuing to provide high-level care amid extremely challenging conditions. She finds it in the positive comments nurses give each other. She finds it in the opportunity to care for others when they need it most.
She holds out hope, too, for the pending development of a vaccine that will protect people against COVID-19, for reduced stress on her nurses, and for a time when friends and family can gather together once again.
“It’s feeling like an ultramarathon right now,” White said. “We know tough times are ahead. But we will get through this. We just need to maintain hope.”
Politics
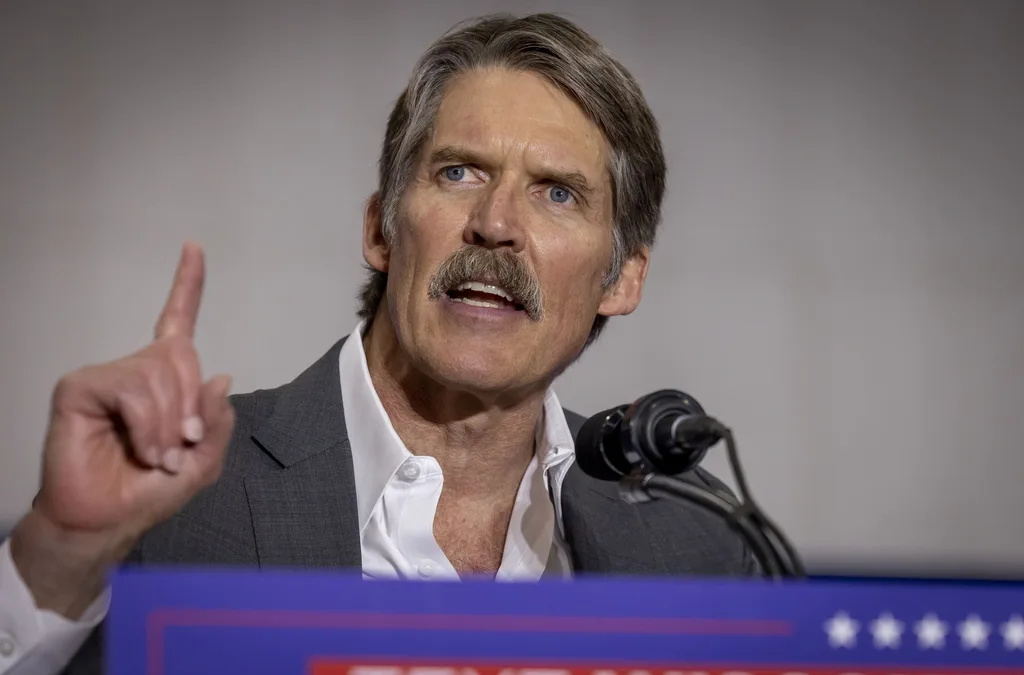
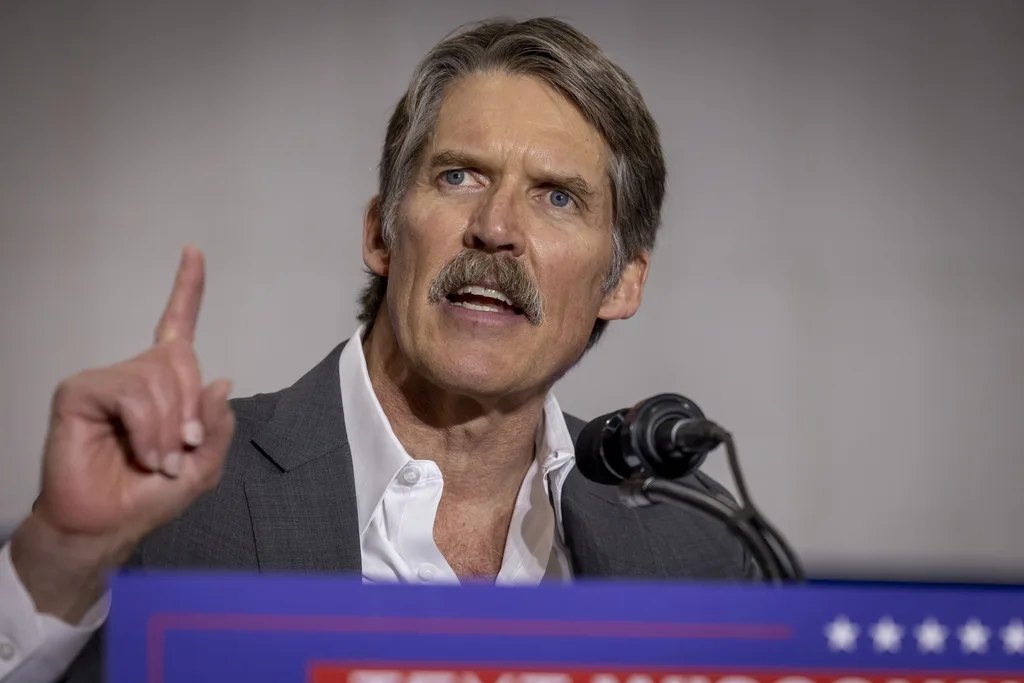
Eric Hovde’s company exposed workers to dangerous chemicals, OSHA reports say
A Madison-based real estate company run by Wisconsin US Senate candidate Eric Hovde settled with the Occupational Safety and Health Administration...

Plugged in: How one Wisconsin school bus driver likes his new electric bus
Electric school buses are gradually being rolled out across the state. They’re still big and yellow, but they’re not loud and don’t smell like...
Local News

Stop and smell these native Wisconsin flowers this Earth Day
Spring has sprung — and here in Wisconsin, the signs are everywhere! From warmer weather and longer days to birds returning to your backyard trees....

Your guide to the 2024 Blue Ox Music Festival in Eau Claire
Eau Claire and art go hand in hand. The city is home to a multitude of sculptures, murals, and music events — including several annual showcases,...