#image_title
#image_title
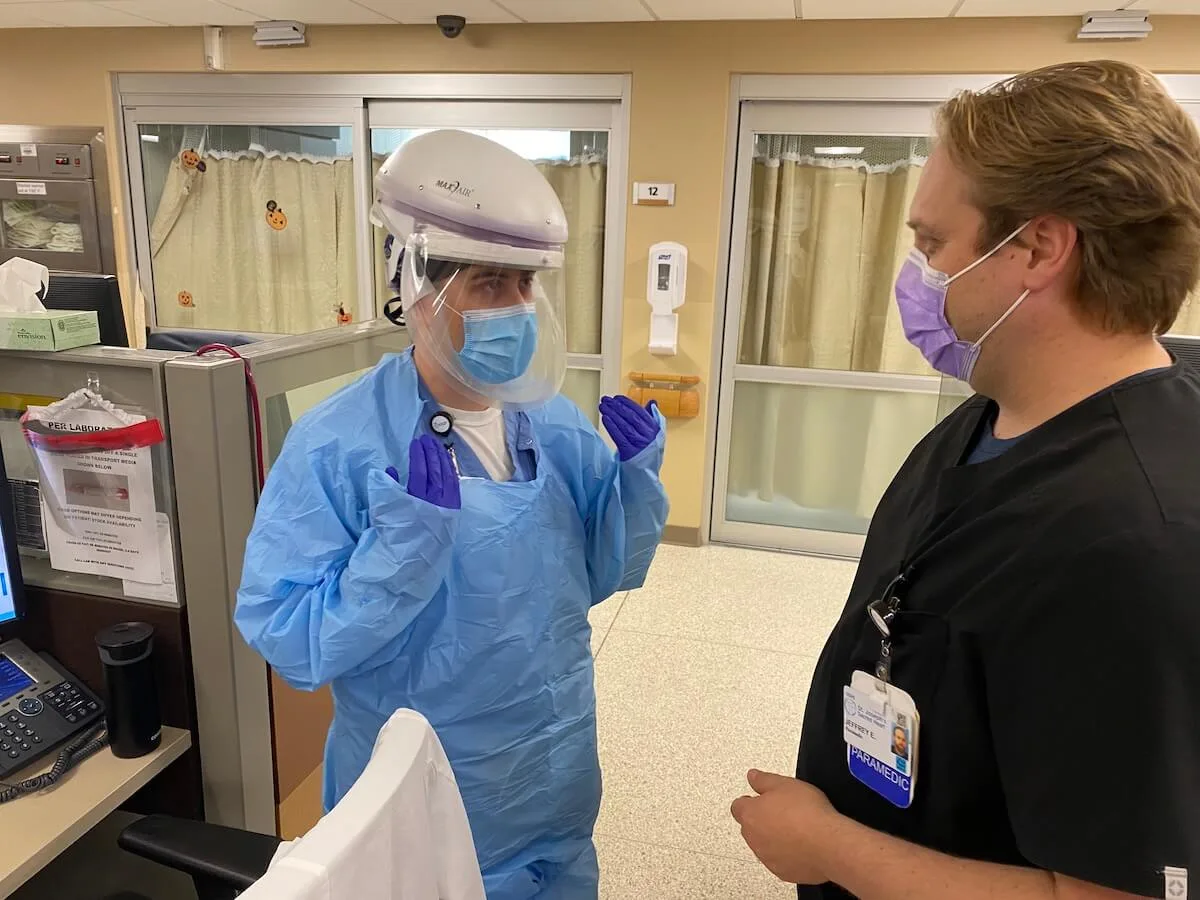
Hospitals across the state are running out of intensive care beds, as new COVID-19 cases again top more than 7,000 in a single day.
As coronavirus cases continue to surge across Wisconsin and overwhelm hospitals, Wisconsin Department of Health Services Chief Medical Officer Dr. Ryan Westergaard said the state has reached a “tipping point” in determining whether significantly more people will die from the virus in upcoming months.
Record numbers of people being infected with the coronavirus are filling hospitals to capacity, and if those totals continue to climb as they have in recent weeks, hospitals may no longer be able to provide the medical care to keep them alive, Westergaard said Wednesday during a COVID-19 panel discussion put on by Wisconsin Health News.
“Right now, our biggest concern is [making sure] that hospitals have the resources to treat people,” Westergaard said when asked about the most serious impact of rapidly rising COVID-19 cases. “We’re close to a tipping point. And that tipping point is when we stop being able to save people.”
On Wednesday 7,048 new COVID-19 cases were reported in Wisconsin, marking the second consecutive day above 7,000, after a one-day record 7,073 on Tuesday. The total is the third-highest for one day, behind Tuesday’s number and 7,065 on Saturday.
Sixty-two new deaths related to COVID-19 also were reported Wednesday, one day after a record 66 people died from the virus. In all, 285,891 cases have been reported and 2,457 people have died from the virus in Wisconsin.
As a sign of the serious nature of Wiconsin’s COVID-19 situation, Gov. Tony Evers on Tuesday issued an executive order urging people to stay home to slow the spread of the virus. He didn’t legally require that action after the state Supreme Court, at the urging of Republicans, overturned an extension of the safer-at-home order in May.
During a televised address, Evers once again urged Wisconsinites to wear masks in public, maintain social distancing, and refrain from gathering with others to spread the virus. On Wednesday, Westergaard did the same, saying those behaviors are the best way to contain COVID-19.
“We haven’t done enough to stop [the virus] by limiting our contact with people,” Westergaard said.
As COVID-19 totals have climbed, so too have the number of people infected with the virus who require hospitalization. On Wednesday 277 new COVID-19 patients were hospitalized in Wisconsin, one day after a record 291.
The influx of COVID-19 patients is leaving hospitals with limited bed space to treat patients. Hospitals across the state report little to no remaining medical-surgical and intensive care beds, forcing them to find alternative spaces to treat patients.
According to Wisconsin Hospital Association figures, just two of 72 intensive care beds at a combined 26 hospitals in the northwest part of the state were immediately available. Sixty-three of 673 medical-surgical beds in the region were available, those statistics show.
Likewise, in central Wisconsin, seven of 128 intensive care beds are available. Other parts of the state show bed shortages too. In the northeast region, just 15 of 207 intensive care beds are available, and 64 of 656 in southeast Wisconsin.
In Eau Claire, a city of 70,000 in west-central Wisconsin, all three major hospitals report being at or near capacity as the number of people infected with COVID-19 requiring hospitalization has skyrocketed in recent weeks, with test-positivity rates for the virus sometimes exceeding 40%.
Mayo Clinic Health System officials said none of the system’s intensive care and medical-surgical beds are available at its Eau Claire, Menomonie, Barron, Bloomer, and Osseo sites. As of late Tuesday, 83 COVID-19 patients were hospitalized at those sites.
Similarly, all medical surgical beds at Marshfield Medical Center-Eau Claire’s 44-bed hospital were full Wednesday morning, although the hospital’s surge plan includes other space to treat patients. Officials at HSHS Sacred Heart Hospital in Eau Claire and HSHS St. Joseph’s Hospital in Chippewa Falls said those facilities also are near capacity and are expecting to admit more COVID-19 patients as virus numbers continue to rise.
All three hospitals said they are treating other patients in addition to those associated with COVID-19. But doing so has become increasingly challenging as those infected with the virus stretch resources.
“The public needs to treat COVID-19 as the health emergency it is to prevent the health care system from being overwhelmed,” Mayo Clinic Regional Vice President Dr. Richard Helmers, Regional Chair of Administration Jason Craig, and Chief Nursing Officer Pam White said in a joint statement.
Bed space isn’t the only shortage at hospitals caused by COVID-19, said Eric Borgerding, chief operating officer of the Wisconsin Hospital Association. Increased spread of the virus means more hospital staff are exposed to it, and hospital officials report significant numbers of nurses and other staff being quarantined and unavailable to treat patients. Some hospitals report as much as 15% of their staff is in quarantine.
“Capacity is being stressed everywhere,” he said.
In De Pere, Sara Lornson, one of three contact tracers working for the city, said they are having trouble keeping up with the growing number of cases.

“We’re behind. We’re very behind in contact tracing,” Lornson said during a virtual press conference Wednesday. “We’re doing our very best and just trying to make a difference and trying to have some impact on those people [they are able to reach].”
Kirsten Johnson said she and her colleagues at the Washington Ozaukee Public Health Department are doing their best to contain COVID-19 and prevent hospitals from filling with patients. But disease spread has far outgrown the ability of her department and other county health officers around Wisconsin to manage.
Johnson, director of her department, said she and other health officials statewide lack the resources to conduct contact tracing, a means of tracking who has the virus and who they have been in contact with. COVID-19 has spiraled so rapidly, she said, that she can’t begin to keep up with contact tracing despite having added 60 workers for that job.
“I am fearful for our healthcare systems if we don’t get a better handle on this,” she said.
Politics

Biden administration bans noncompete clauses for workers
The Federal Trade Commission (FTC) voted on Tuesday to ban noncompete agreements—those pesky clauses that employers often force their workers to...

Opinion: Trump, GOP fail January 6 truth test
In this op-ed, Milwaukee resident Terry Hansen reflects on the events that took place on January 6, the response from Trump and other GOP members,...
Local News

Readers Poll: Top Bowling Alleys in Wisconsin
Looking for the best bowling in Wisconsin? Look no further! Our readers have spoken in our recent poll, and we have the inside scoop on the top...

8 Wisconsin restaurants Top Chef judges are raving about
Top Chef’s 21st season is all about Wisconsin, and on-screen, it’s already apparent that the judges feel right at home here. But, while filming in...