#image_title
#image_title
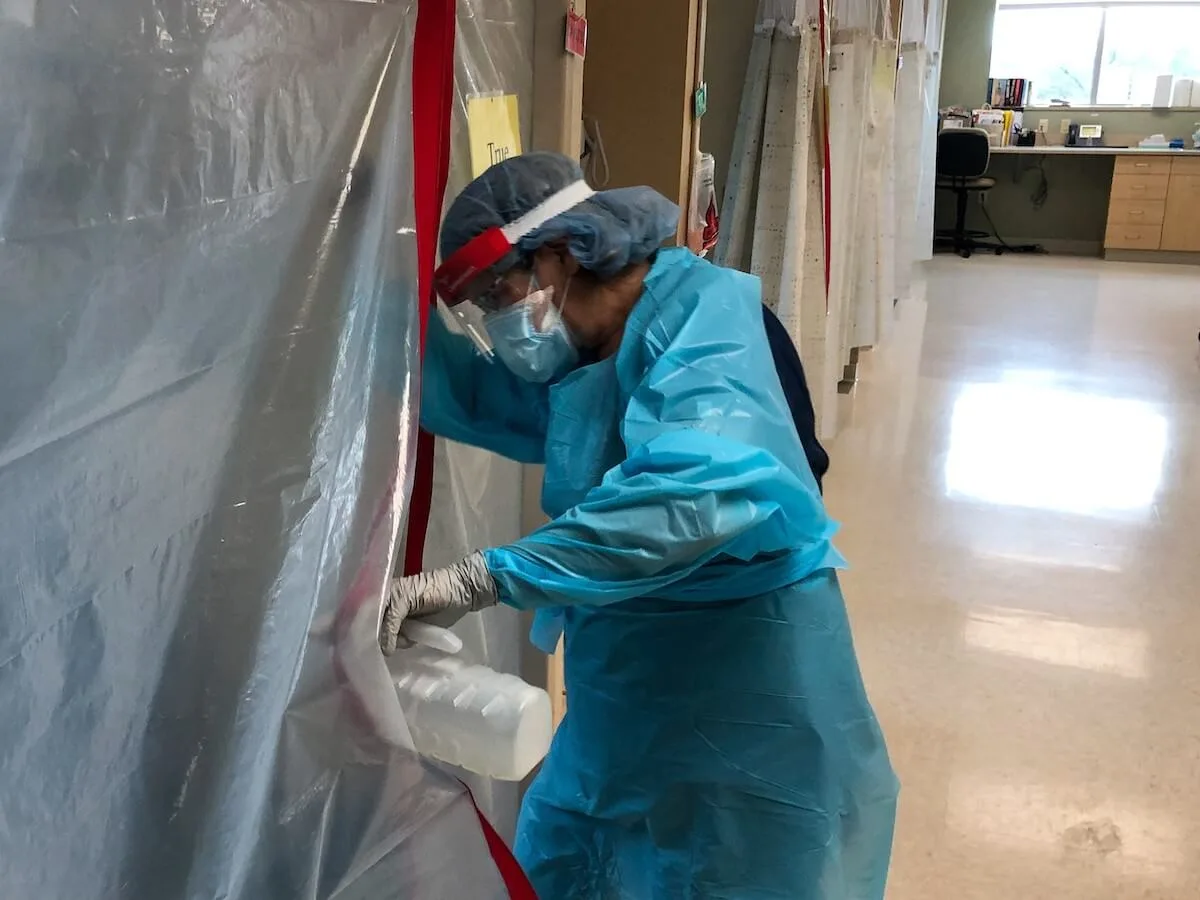
COVID-19 includes lingering symptoms months after testing positive, to isolated stays in intensive care units, separated from loved ones.
De Pere Mayor James Boyd was talking on the phone with the city’s health director when he coughed a little bit.
“She asked, ‘What was that?’” said Boyd during a virtual conference on COVID-19 Wednesday hosted by the Brown County Health Department.
Boyd had a runny nose, a bit of cough, some body aches and fatigue. But he didn’t think it was serious enough to be concerned.
“I wasn’t really thinking of getting tested because it didn’t seem that severe,” he said.
At the advice of the health director he got tested. On Sept. 24, he was diagnosed with COVID-19. No one else he had associated with was positive, and he always wore a mask when he left the house. To this day, he doesn’t know how he got it.
At first he thought he was going to be one of the lucky ones because his symptoms were so mild. But a few days later, the disease really ramped up.
He experienced nausea so severe he found food and drink repulsive. He lost his sense of taste and smell. His body was in pain. One leg hurt so bad it was difficult for him to fall asleep. He said he had about 11 or 12 of the symptoms listed for COVID-19 and was sick for 12 to 14 days.
“I was very, very, very sick,” he said.
A friend gave him a pulse oximeter—a device that measures blood oxygen levels—which he kept checking as his symptoms got worse. Despite how bad he felt, he never needed to be hospitalized.
“I figure I got pretty close because that’s the sickest I’ve ever been,” he said.
Over two months later, he is just starting to recover his sense of taste but his sense of smell is still gone. He still feels tightness in his chest and experiences bouts of fatigue.
“I have not had a quality of life since it started,” Boyd said. “People need to realize that there are a lot of people like me. We are not recovered.”
Boyd spoke at the “Faces of COVID” media event to spread awareness about how, even in a best-case scenario, the virus is not to be taken lightly. He directly addressed people who continue not to take the pandemic seriously or take precautionary measures against spreading the virus.
“If they have any compassion or sympathy for those they love, they have to take this seriously,” Boyd said. “We’re not done. We’re not even close to being done.”
ICU isolation
The line between being able to recover at home and needing to go to the hospital, is often drawn at whether a patient feels short of breath, Dr. Brad Burmeister with Bellin Health said. But it’s not the only symptom.
Burmeister said patients who lose their sense of smell or taste may experience an aversion to food and drink and become dehydrated, which can also be cause for concern. The combination of hypoxia from a lack of oxygen and dehydration can also lead to motor control issues that can lead to people injuring themselves.
If a COVID-19 patient is admitted, they have a very different and very difficult experience from other intensive care patients, said Dr. Syed Shah with Aurora BayCare Medical Center.
“The normal routine for patients admitted into the ICU, they have family around. For the majority of these [COVID-19] patients they don’t have family that can come and be there with them,” he said. “We try our best to support them in terms of emotional support and hope.”
It’s especially hard for patients who are dying, as well as their families, nurses, and physicians.
“That is the time when the family should be there,” he said. “There is not a lot we can do for terminal patients. We try to get the family in there to see them and say their goodbyes. It is still traumatic at the end.”
The fortunate ones
For those who are fortunate enough to recover, the side effects from the virus can linger for weeks, even months.
Dr. David Palubiak with HSHS St. Mary’s and HSHS St. Vincent Hospital said the spectrum for how people remain hospitalized is very broad, anywhere from five to 14 days.
Once patients are discharged, they receive instructions on how long to quarantine, how to check their vitals, worsening symptoms to watch out for and what to do if breathing becomes more difficult, and when they should return to the hospital.
“The amount of discharge instruction is very intense when they’re going home,” he said.
He is finding that many patients who are discharged return to the hospital weeks later. For example, patients who are diabetic or have heart disease before contracting COVID-19 will experience new problems managing those conditions afterward.
Some patients will return with new conditions they didn’t have before, such as heart problems, blood clots, organ issues caused by blood clots, lung infections, lung scarring and ongoing breathing problems. One patient would pass out when they stood up. And many say they still experience mental fog.
“There’s almost anything you can imagine,” Palubiak said.
Politics
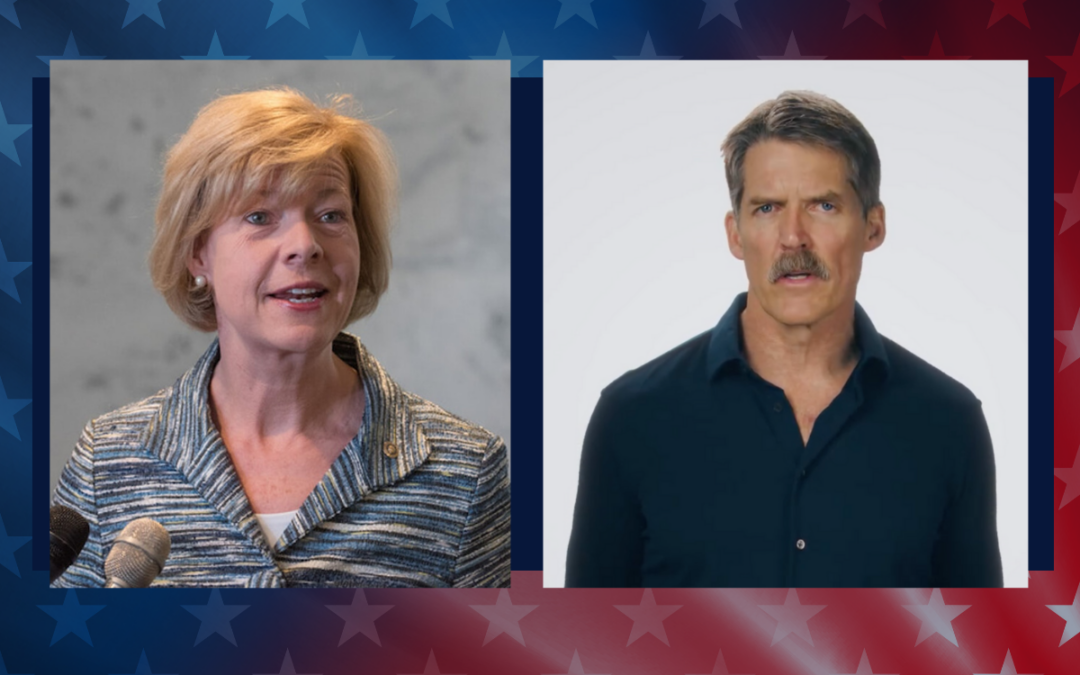
What’s the difference between Eric Hovde and Sen. Tammy Baldwin on the issues?
The Democratic incumbent will point to specific accomplishments while the Republican challenger will outline general concerns he would address....

Who Is Tammy Baldwin?
Getting to know the contenders for this November’s US Senate election. [Editor’s Note: Part of a series that profiles the candidates and issues in...
Local News

Stop and smell these native Wisconsin flowers this Earth Day
Spring has sprung — and here in Wisconsin, the signs are everywhere! From warmer weather and longer days to birds returning to your backyard trees....

Your guide to the 2024 Blue Ox Music Festival in Eau Claire
Eau Claire and art go hand in hand. The city is home to a multitude of sculptures, murals, and music events — including several annual showcases,...


